Acquired Brain Injury: Are We Doing Enough?
Acquired Brain Injury (ABI), Traumatic Brain Injury (TBI), and Chronic Traumatic Encephalopathy (CTE) and Their Relationship to Domestic Violence
Paula Ciniero, the owner of Healing Hands Healing Hearts in Fairbanks, AK, was a registered nurse for almost 40 years and an energy worker working within the body’s energy systems and biofield. She is a certified Healing Touch Practitioner, Reiki Master, and CranioSacral Practitioner trained in other complementary medical services. She is also a certified sound healer specializing in crystal singing bowls and Himalayan bowl therapy. Paula has had various experiences in all realms of the nursing profession. Paula has also worked as a health nurse in rural Alaska for many years.
In working with survivors of domestic violence (DV), Paula has been able to feel the cold and emptiness in one part of the brain and warmth and fullness in the other parts. One particular survivor had been thrown down the stairs and had suffered a brain hematoma (large brain bruise). Where the survivor had the hematoma, Paula felt the cold and emptiness.
While we are unsure about the exact numbers of head injuries related to DV in the Indigenous population in the US and its territories, we understand that there is a definitive connection and relationship between Acquired Brain Injury (ABI), Chronic Traumatic Encephalopathy (CTE), Traumatic Brain Injury (TBI), and their relationship to DV. Medical Journal searches, such as through PubMed and the NIH, show numerous studies on combat veterans but very few on the impacts on US Indigenous populations.
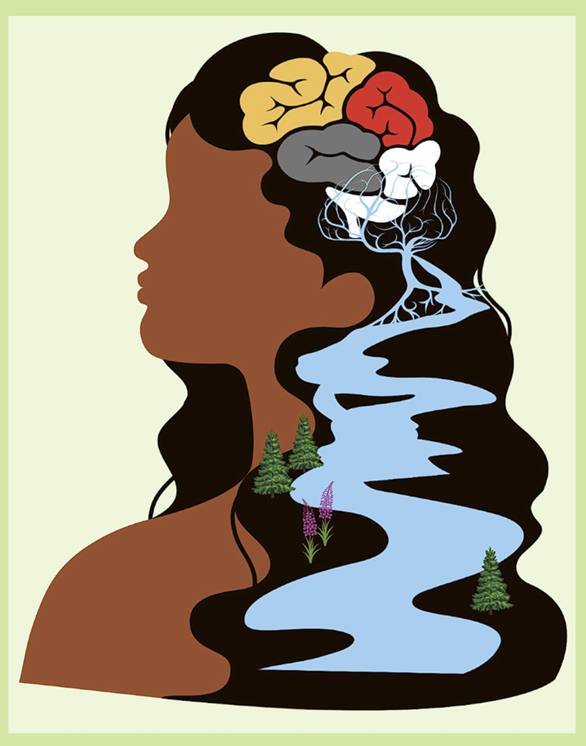
Acquired brain injury (ABI) is a term used for internal (non-traumatic) and external (traumatic) brain injury. Nontraumatic brain injury causes damage to the brain by internal factors, such as a lack of oxygen, exposure to toxins, pressure from a tumor, etc. A traumatic brain injury (TBI) is an alteration in brain function caused by an external force on the head, such as falls, vehicle accidents, explosions, or violence.
TBI can cause severe symptoms and long-term etiology. Severe symptoms can include loss of consciousness, confusion, disorientation, seizures, numbness or weakness of the extremities, nausea, vomiting, dizziness, slurred speech, trouble walking, and blood or clear fluid coming from the nose or ears. If a person is experiencing these, they must get to a clinic or medical center immediately. In our Villages and on Reservations, medical care is often a long way away, and the survivor does not always visit the local clinic to be seen once this happens. There are several reasons for this. The partner does not allow her to get medical attention. She wants to curl up and forget the trauma. Medical care is too far away, and clinic staff may be related to the perpetrator. They may also fear child removal, escalating violence, prioritization of other injuries or competing demands, and insufficient awareness of the signs of brain injury. They may be afraid to leave the children or pets with their partner while they seek medical attention.
With any TBI, what is most concerning for all survivors who experience physical violence from their partners is whether or not all survivors have access to and are receiving medical attention to mitigate the long-term effects of any head injury. Before we discuss some of those effects, let’s talk about chronic traumatic encephalopathy (CTE).
CTE is a term given to brain injuries that occur in professional football players and now in professional hockey players. Brain injury occurs from repeated blows to the head sustained in football games and practice. The career of a professional football player is around 26 years. A survivor can be in a relationship experiencing DV for 40 years, including repeated instances of head trauma.
Some of the long-term effects of both TBI and CTE include concentration and memory problems, delayed thinking and understanding, headaches, seizures, vision changes, fatigue, balance problems, mood swings, reduced language skills, problemsolving challenges, poor planning and judgment, lack of impulse control, depression, anxiety, sleep disturbances. Not all those with brain injury or CTE have all of these, and some will come and go, but they do lead to a multitude of other issues.
TBI and CTE may lead to challenges for survivors during forensic interviewing, such as concentration and memory problems, as well as delayed thinking and understanding. Additionally, many survivors may be labeled as non-compliant because they do not show up for appointments. They just may not remember, especially if it is not written down for them.
Our autonomic nervous system has two parts: Sympathetic (fight, flight, freeze, fawn) and Parasympathetic (rest, digest). These two systems allow people to respond to various situations. In normal circumstances, our sympathetic nervous systems rev up when a threat occurs. For instance, a bear starts to chase us, our heart rate speeds up, our breathing becomes rapid, our muscles engage, our stomach tightens, and we flee to our car. Once in our car, our heart rate and breathing slow, our stomach unclenches, and we settle down. Persons with TBI can experience sympathetic nervous system dominance and, in some cases, parasympathetic dominance, and it could swing back and forth. No one knows yet why this happens, but it can cause a wide scope of problems within the physical body.
Although more research and evaluation is needed, especially as it relates to our U.S. Indigenous populations, there is an undeniable connection between CTE, TBI, and ABI, especially as it relates to DV survivors and survivors of all gender-based violence. Initial and ongoing education and training for advocates, first responders, health care professionals, and others who interact with survivors will be critical in navigating the too often untreated, complex responses and behaviors of DV survivors.
![]()
Traumatic Brain Injury Booklet
• Go to: bit.ly/4dDLrwb
NIWRC Webinars
• Go to: bit.ly/3V2eClp